Practice Policies & Patient Information
Carbon Reduction Plan
Carbon Reduction Plans are to be completed by the bidding supplier entity and must meet the reporting requirements set out in supporting guidance, and include the supplier’s current carbon footprint and its commitment to reducing emissions to achieve Net Zero emissions by 2050.
- The Carbon Reduction Plan should be:-
- updated regularly (at least annually)
- published and clearly signposted on the supplier’s UK website.
- approved by a director (or equivalent senior leadership) within the supplier’s organisation to demonstrate a clear commitment to emissions reduction at the highest level.
Suppliers may wish to adopt the key objectives of the Carbon Reduction Plan within their strategic plans.
Procurement Policy Note 06/21: Taking account of Carbon Reduction Plans in the procurement of major government contracts – GOV.UK (www.gov.uk)
Publication date: 7th March 2025
Commitment to achieving Net Zero
Premium Wipes and Textiles Limited is committed to achieving Net Zero emissions by 2050.
Baseline Emissions Footprint
Baseline emissions are a record of the greenhouse gases that have been produced in the past and were produced prior to the introduction of any strategies to reduce emissions. Baseline emissions are the reference point against which emissions reduction can be measured.
| Baseline Year: 2024 – we have not previously reported on our emissions. We have estimated our emissions from 2024 and will use this as our baseline to measure progress against reducing our carbon emissions. |
| Additional Details relating to the Baseline Emissions calculations. |
| As this is the first operational year for Spirit Primary Care Limited, no prior emissions reporting has been conducted. Therefore, the 2023-24 baseline has been established to align with the requirements under this measure.
– Scope 1 and Scope 2 Emissions: Calculations for direct emissions (Scope 1) and energy-related emissions (Scope 2) have been conducted using data from energy usage, fleet operations (which is not applicable), and other relevant sources. – Scope 3 Emissions: This baseline year also includes a newly created reporting structure for Scope 3 emissions, which incorporates supply chain activities, waste generation, and employee commuting. Historical data for Scope 3 emissions are unavailable due to the absence of prior reporting requirements. The creation of this baseline reflects organisational change, including the establishment of BWPCA as a distinct operational entity. Moving forward, this baseline will be used to track and manage emissions reductions in line with net zero targets. |
| Baseline year emissions: | |
| EMISSIONS | TOTAL (tCO2e) |
| Scope 1 | N/A (no direct emissions due to lack of fleet or fuel use/not relevant for the organisation) |
| Scope 2 | 25 tCO2e |
| Scope 3 (Included Sources) |
40 tCO2e (e.g., waste generation, staff commuting, and procurement of medical supplies) |
| Total Emissions | 65 tCO2e |
Current Emissions Reporting
| Reporting Year: 2025 – we currently do not report on our emissions. Our baseline year is 2024 with data for our 2025 emissions to be reported at the end of this year. | |
| EMISSIONS | TOTAL (tCO2e) |
| Scope 1 | N/A (no direct emissions due to lack of fleet or fuel use/not relevant for the organisation) |
| Scope 2 | 22 tCO2e (reflecting energy efficiency upgrades) |
| Scope 3 (Included Sources) |
38 tCO2e (reflecting minor operational changes). |
| Total Emissions | 60 tCO2e |
Emissions reduction targets
To achieve Net Zero by 2050, we have adopted the following interim reduction targets:
- By 2030: Reduce emissions by 30% to 45 tCO2e.
- By 2040: Reduce emissions by 70% to 20 tCO2e.
These targets will be reviewed annually, and progress will be reported publicly on the organisation’s website.
Carbon Reduction Projects
Completed Initiatives:
Since the baseline year (2024), we have implemented the following measures to reduce its carbon footprint:
- Staff Education: We have introduced “carbon reduction plans” at induction and have engaged staff feedback to identify additional opportunities.
- Sustainable Travel: We encourage public transport, walking, cycling, and car sharing; as well as register with the Bike2Work Scheme and track participation via travel expense claims.
- Remote Working: We support remote working and hold meetings via MS Teams to reduce travel emissions.
- Paper Reduction: We have increased reliance on digital records and electronic communications, monitored through reductions in postage, ink, and paper costs.
- We maximise EPS usage.
- Water Conservation: We are working with stakeholders to implement water-saving measures, tracked via reduced water bills.
- Local and Green Suppliers: We actively prioritise local suppliers with green credentials to reduce transportation emissions.
- We are educating staff to reduce single-use plastics and waste.
- We are monitoring reductions in black-bin refuse and increasing recycling rates.
- Across the constituent member practices, we have transitioned 60% of patient communication to digital platforms (e.g., text messaging, patient portals), reducing reliance on paper-based methods.
Future Projects:
To further progress towards Net Zero, we plan to:
- Work with stakeholders to achieve a 60% transition to renewable energy sources for electricity consumption in practice buildings
- Work with stakeholders to improve water-saving measures, such as low-flow taps, in facilities.
- Increase digital transformation efforts, including further adoption of paperless record-keeping.
- Continue to engage staff and patients in sustainability initiatives through awareness campaigns.
Declaration and Sign Off
This Carbon Reduction Plan has been completed in accordance with PPN 06/21 and associated guidance and reporting standard for Carbon Reduction Plans.
Emissions have been reported and recorded in accordance with the published reporting standard for Carbon Reduction Plans and the GHG Reporting Protocol corporate standard1 and uses the appropriate Government emission conversion factors for greenhouse gas company reporting2
Scope 1 and Scope 2 emissions have been reported in accordance with SECR requirements, and the required subset of Scope 3 emissions have been reported in accordance with the published reporting standard for Carbon Reduction Plans and the Corporate Value Chain (Scope 3) Standard3
This Carbon Reduction Plan has been reviewed and signed off by the board of directors (or equivalent management body).
1 https://ghgprotocol.org/corporate-standard
2 https://www.gov.uk/government/collections/government-conversion-factors-for-company-reporting
3 https://ghgprotocol.org/standards/scope-3-standard
Chaperone Policy
It is a requirement that, when necessary, chaperones are provided to protect and safeguard both patients and clinicians during intimate examinations and or procedures.
1 Introduction
1.1 Policy Statement
It is a requirement that, when necessary, chaperones are provided to protect and safeguard both patients and clinicians during intimate examinations and or procedures.
All clinical and non-clinical staff may at some point be asked to act as a chaperone at this organisation. Therefore, it is essential that training is given and trained chaperones are aware of their individual responsibilities when performing chaperone duties.
The CQC GP Mythbuster 15: Chaperones advises that for children and young people, their parents, relatives and carers should be made aware of the policy and why this is important.
To raise awareness, the chaperone policy should be clearly advertised. At this organisation, a chaperone poster is clearly displayed in the waiting area, in all clinical areas and annotated in the organisation leaflet as well as on the organisation website.
1.2 Status
The organisation aims to design and implement policies and procedures that meet the diverse needs of our service and workforce, ensuring that none are placed at a disadvantage over others, in accordance with the Equality Act 2010. Consideration has been given to the impact this policy might have regarding the individual protected characteristics of those to whom it applies.
This document and any procedures contained within it are non-contractual and may be modified or withdrawn at any time. For the avoidance of doubt, it does not form part of your contract of employment. Furthermore, this document applies to all employees of the organisation and other individuals performing functions in relation to the practice such as agency workers, locums and contractors.
2 Policy
2.1 Who can act as a chaperone
The GMC Intimate examinations and chaperones guidance explains that the patient should be given the option of having an impartial observer (a chaperone) present whenever possible.
As per the GMC guidance, relatives or friends of the patient are not considered to be an impartial observer so would not usually be a suitable chaperone but staff at this organisation should comply with a reasonable request to have such a person present in addition to the chaperone.
It is policy that any member of the organisation team can act as a chaperone only if they have undertaken appropriate chaperone training as detailed in CQC GP Mythbuster 15.
Additionally, all staff must complete chaperone awareness training which covers the role of the chaperone.
2.2 General guidance
The GMC guidance states that before conducting an intimate examination, the clinician should:
- Explain to the patient why the particular examination is necessary and give the patient the opportunity to ask questions
- Explain what the examination will involve, in a way the patient can understand, so that the patient has a clear idea of what to expect including any pain or discomfort
- Get the patient’s permission before the examination and record that the patient has given it
- Offer the patient a chaperone
- If dealing with a child or young person:
- Assess their capacity to consent to the examination
- If they lack the capacity to consent, seek parental consent
- Give the patient privacy to undress and dress and keep them covered as much as possible to maintain their dignity; they should not help the patient to remove clothing unless they have been asked to or they have checked with the patient that they want help
During the examination, the clinician should:
- Explain what they are going to do before they do it, and if this differs from what they previously told the patient, explain why and seek the patient’s permission
- Stop the examination if the patient asks them to
- Keep discussion relevant and not make unnecessary personal comments
When a chaperone is present, the details of the chaperone must be recorded in the patient’s clinical record.
2.3 Expectations of a chaperone
At this organisation, chaperones will adhere to the GMC guidance which states chaperones will:
- Be sensitive and respect the patient’s dignity and confidentiality
- Reassure the patient if they show signs of distress or discomfort
- Be familiar with the procedures involved in a routine intimate examination
- Stay for the whole examination and be able to see what the doctor is doing, if practical
- Be prepared to raise concerns if they are concerned about the doctor’s behaviour or actions
The CQC advises that for most patients and procedures, respect, explanation, consent and privacy are all that are needed. These take precedence over the need for a chaperone. A chaperone does not remove the need for adequate explanation and courtesy. Neither can a chaperone provide full assurance that the procedure or examination is conducted appropriately.
2.4 When a chaperone is unavailable
The GMC advises that if either the clinician or the patient does not want the examination to go ahead without a chaperone present, of if either is uncomfortable with the choice of chaperone, the clinician may offer to delay the examination until a later date when a suitable chaperone will be available as long as the delay would not adversely affect the patient’s health.
2.5 When a patient refuses a chaperone
If the clinician does not want to proceed with the examination without a chaperone but the patient has refused a chaperone, the clinician must clearly explain why they want a chaperone present. The GMC states that ultimately the patient’s clinical needs must take precedence. The clinician may wish to consider referring the patient to a colleague who would be willing to examine them without a chaperone as long as a delay would not adversely affect the patient’s health.
Any discussion about chaperones and the outcome should be recorded in the patient’s medical record, and in particular:
- Who the chaperone was
- Their title
- That the offer was made and declined
2.6 Disclosure and Barring Service (DBS) check
Clinical staff who undertake a chaperone role at this organisation will already have a DBS check. The CQC states that non-clinical staff who carry out chaperone duties may need a DBS check. This is due to the nature of chaperoning duties and the level of patient contact. Should the organisation decide not to carry out a DBS check for any non-clinical staff, then a clear rationale for this decision must be given including an appropriate risk assessment.
2.7 Using chaperones during a video consultation
CQC GP Mythbuster 15 explains that many intimate examinations will not be suitable for a video consultation. When online, video or telephone consultations take place, GMC guidance explains how to protect patients when images are needed to support clinical decision making. This includes the appropriate use of photographs and video consultations as part of patient care.
When intimate examinations are performed, it is important that a chaperone is offered. Documentation should clearly reflect this. It is important to document who provided the chaperoning and this should also state what part of the consultation they were present for.
This guidance explains how to conduct intimate examinations by video and the use of chaperones.
2.8 Practice procedure (including SNOMED codes)
If a chaperone was not requested at the time of booking the appointment, the clinician will offer the patient a chaperone explaining the requirements:
- Contact reception and request a chaperone
- Record in the individual’s healthcare record that a chaperone is present and identify them
- The chaperone should be introduced to the patient
- The chaperone should assist as required but maintain a position so that they are able to witness the procedure/examination (usually at the head end)
- The chaperone should adhere to their role at all times
- Post procedure or examination, the chaperone should ensure they annotate in the patient’s healthcare record that they were present during the examination and there were no issues observed
- The clinician will annotate in the individual’s healthcare record the full details of the procedure as per current medical records policy
| Detail | SNOMED CT Code |
|---|---|
| The patient agrees to chaperone | 1104081000000107 |
| Refusal to have a chaperone present | 763380007 |
| No chaperones available | 428929009 |
2.9 Escorting of visitors and guests (including VIPs)
There may be, on occasion, a need to ensure that appropriate measures are in place to escort visitors and guests including VIPs. On such occasions, this organisation will follow the recommendations outlined in the Lampard Report (2015).
If media interest is likely, the Practice Manager is to inform the local ICB, requesting that the communication team provides guidance and/or support where necessary
Confidentiality
Under the Data Protection Act 2018 you have a right to know who holds personal information about you. This person or organisation is called the data controller. In the NHS, the data controller is usually your local NHS board and your GP surgery. The NHS must keep your personal health information confidential. It is your right.
Please be aware that our staff are bound to the NHS code of confidentiality. Our staff are therefore not permitted to discuss any of our patient’s medical history, this includes their registration status, without their written consent to do so.
Once we have received their written consent and verified this with the patient, then we can provide you with this information, this includes complaining on behalf of a patient, but excludes patients who are unable to act on their own behalf and already have a designated person or carer responsible for their medical care.
We therefore respectfully ask parents and guardians not to request information regarding their relatives or to complain on their behalf unless we have their written consent to do so.
Entitlement to NHS Treatment
The NHS is the UK’s state health service which provides treatment for UK residents. Some services are free, other have to be paid for. The regulations that govern who can and can’t receive treatment are complex and may change.
A person who is regarded as ordinarily resident in the UK is eligible for free treatment by a GP. A person is ‘ordinarily resident’ for this purpose if lawfully living in the UK for a settled purpose as part of the regular order of his or her life for the time being. Anyone coming to live in this country would qualify as ordinarily resident. Overseas visitors to the UK are not regarded as ordinarily resident if they do not meet this description.
The following NHS treatment is available to anyone:
- Treatment in an emergency (but not follow up treatment).
- Treatment of certain communicable diseases.
- Compulsory psychiatric treatment.
To qualify for other NHS treatments you must meet certain conditions which are outlined below.
EU Nationals
Foreign nations from EU member states have reciprocal arrangements for both dental and medical healthcare so can access the full range of NHS services.
Non EU nationals
Foreign nationals from non-EU countries have no automatic right to NHS healthcare (other than those outlined above). Students and visitors who are going to stay in the UK for less than 6 months would have to be seen as private patients and would have to pay for their treatment. It is therefore essential that you have medical insurance to pay for any private treatment.
If you are not a student registered at a UK university and you are not going to stay in the UK for between six months and a year, it may be unlikely that you will be able to receive free NHS Treatment.
If you are unsure of entitlement to NHS treatment, or require further information please ask the reception staff when you register, and they will advise you accordingly.
Be aware that a valid 6 month visa does not automatically confer the right to free NHS treatment.
Please note that registering with a GP does not give you automatic entitlement to access free NHS hospital treatment. It is therefore essential that you take out medical insurance for the duration of your visit prior to arrival in the UK.
If you are a student registered at a UK University (and you have documentary proof of this) and are going to stay in the UK for more than six months you will qualify for NHS treatment from the beginning of your stay and you (and your dependants) will be entitled to NHS treatment and you may register with a GP.
Medical emergencies
If you need immediate medical assistance (e.g. because of an accident) telephone 999 – the call is free. An operator will ask you which emergency service you require (fire, police or ambulance). You will need to tell the emergency services what has happened and where you are. If someone is injured and needs to go to hospital an ambulance will arrive and take them to the nearest hospital with an emergency department
If you need urgent treatment but are well enough to travel please make your own way to the nearest Accident and Emergency Department.
GDPR and Data Protection
We use your information to provide you with Health Care services, and share your information with other organisations involved in your care.
We do this under Article 6(1) and Article 9(2)(h) of the GDPR.
You are entitled to see what information we hold about you on request.
How you can help us
- Please keep the appointment or cancel it well in advance to allow other people to see us
- Please book urgent appointments for emergencies only
- If you feel you need a longer appointment for your problem, please tell reception at the time of booking the appointment
- If you change your name, address or telephone number please inform us as soon as possible
- Only call the Doctor out of hours if you can’t wait
- Be polite to the staff as they are just doing their job
- The practice operates a zero tolerance policy, any patient that is violent or abusive to any member of staff may risk being removed from the practice list
Medical Research
Information in patient records is important for medical research to develop new treatments and test the safety of medicines. This practice supports medical research by sending some of the information from patient records to the Clinical Practice Research Datalink (CPRD).
CPRD is a Government organisation that provides anonymised patient data for research to improve patient and public health.
You cannot be identified from the information sent to CPRD.
If you do not want anonymised information from your patient record to be used in research you can opt out by speaking to your doctor.
Missed Appointments
A DNA is someone who Did Not Attend an appointment at the surgery and did not tell us beforehand. The Doctor or Nurse were waiting, but the patient did not attend. DNAs are a serious problem for the NHS. Research shows that around 13 million GP appointments and 6 million practice nurse appointments are missed each year.
Due to an increase in the number of wasted appointments through patients failing to attend without informing the practice, it has become necessary to implement the following policy:
- If you fail to attend three appointments without informing us, we will write to you asking if there are any specific problems preventing us from letting us know.
- If you repeatedly fail to attend for appointments, you may be removed from the practice list and have to find an alternative GP practice.
Modern Slavery Policy and Statement
This document is used by all services owned, operated or contracted by Spirit Primary Care Limited (SPCL)
This policy/procedure applies to the following roles:
| Role | Read and follow | Be aware |
|---|---|---|
| Administrative and Support staff | Yes | |
| Clinical staff | Yes | |
| Directors | Yes | |
| Head Office Staff | Yes | |
| Managers | Yes | |
| Other: [add if relevant or leave blank] |
Introduction
This policy applies to all persons working for us or on our behalf in any capacity, including employees at all levels, Directors, Senior Managers, Agency Workers, Locums and Suppliers.
We strictly prohibits the use of modern slavery and human trafficking in our services and supply chain. We have and will continue to be committed to implementing systems and controls aimed at ensuring that modern slavery is not taking place anywhere within our organisation or in any of our supply chains.
We expect suppliers to the same high standards.
Definition
-
- Modern slavery
The Modern Slavery Act 2015 encompasses slavery, human trafficking, forced labour and domestic servitude. Traffickers and slave masters use whatever means they have at their disposal to coerce, deceive and force individuals into a life of abuse, servitude and inhumane treatment.
- Modern slavery
-
- Human Trafficking
Trafficking is the movement of people by means such as force, fraud, coercion or deception with the aim of exploiting them. It is a form of Modern Slavery. People can be trafficked for many different forms of exploitation such as forced prostitution, forced labour, forced begging, and forced criminality, forced marriage, domestic servitude and forced organ removal. Trafficking can occur within the UK as well as countries outside the UK.
- Human Trafficking
Key signs of Modern Slavery and Human Trafficking
Physical
-
- Injuries apparently as a result of assault or controlling measures
-
- Neurological symptoms, headaches, memory loss, dizzy spells
-
- Gastrointestinal symptoms
-
- Cardiovascular symptoms
-
- Musculoskeletal symptoms
-
- Tattoos or other marks indicating ownership by exploiters
-
- Work related injuries, often through inadequate personal protective equipment or poor health and safety measures.
Sexual
-
- Sexually transmitted infections
-
- Injuries of a sexual nature
-
- Gynaecological symptoms such as urinary or virginal infections, pelvic inflammation
-
- Pregnancy as a result of their modern slavery situation, or they may have recently been forced to terminate a pregnancy.
Psychological
-
- Expression of fear or anxiety
-
- Depression or isolation
-
- Suffering from post-traumatic stress and or a range of other trauma induced mental or physical illnesses
-
- An attitude of self-blame, shame and an extensive loss of control
-
- Withdrawn and submissive
-
- Drug or alcohol use
-
- Self-harm
-
- Suicidal ideations.
Pregnancy
-
- Late booking
-
- Frequent non-attendance at appointments
-
- Poor preparation for impending birth
-
- Frequent calls to helpline
-
- Frequent attendances to out of hours services and triage
-
- Presenting with non-specific symptoms
-
- Reluctance to seek help
-
- Poor or no antenatal care
-
- Few personal effects.
Situational and environmental indicators
-
- Frequently moves locations, boroughs, counties, or countries
-
- Fearful or emotional about their family or dependants
-
- Lack of knowledge about the area they live in the UK
-
- Passport or travel document has been confiscated
-
- Fear of saying what their immigration status is
-
- Limited English, e.g., having vocabulary relating only to their exploitative situation
-
- Acting as if instructed by another
-
- Someone is taking advantage of their illegal status in the UK
-
- Distrust of authorities.
General Signs
-
- No passports
-
- No information about rights as a UK worker
-
- No information about their rights as a visitor in the UK
-
- Vague and inconsistent history
-
- Always accompanied by someone who may appear controlling
-
- Person with them does all the talking
-
- Never left alone
-
- Unsure of own medical history
-
- Not registered with a GP, nursery or school
-
- Appearance suggest neglect, note, someone working in prostitution may look well kept.
What to do if you spot the signs
If you suspect that a person is a victim of slavery or trafficking, this is a safeguarding issue.
You should trust and act on your professional instinct that something is not quite right. It is usually a combination of triggers, an inconsistent story and a pattern of symptoms that may cause you to suspect trafficking.
If you have any concerns about a child, young person or adult take immediate action to ask further questions and get additional information and support. It is important to remember that:
-
- trafficked people may not self-identify as victims of modern slavery
-
- trafficking victims can be prevented from revealing their experience to health care staff from fear, shame, language barriers and a lack of opportunity to do so. It can take time for a person to feel safe enough to open up
-
- err on the side of caution regarding age. If a person tells you they are under 18 or if a person says they are an adult, but you suspect they are not, then take action as though they were under 18 years old
-
- support for victims of human trafficking is available.
Action to take
-
- Take immediate action for those considered to be in immediate danger
-
- Follow local safeguarding referral processes
-
- Raise concerns with safeguarding lead
-
- Ensure a clear and accurate record of the concern is made and actions taken.
Policy
Commitments
We are a company that expects everyone working with us or on our behalf to support and uphold the following measures to safeguard against modern slavery and human trafficking:
-
- We have a zero-tolerance approach to modern slavery and human trafficking in our organisation and our supply chains.
-
- The prevention, detection and reporting of modern slavery and human trafficking in any part of our organisation or supply chain is the responsibility of all those working for us or on our behalf. Colleagues must not engage in, facilitate or fail to report any activity that might lead to, or suggest, a breach of this policy.
-
- We are committed to engaging with our stakeholders and suppliers to address the risk of modern slavery and human trafficking in our operations and supply chain.
-
- We take a risk-based approach to our contracting processes and keep them under review. We assess whether the circumstances warrant the inclusion of specific prohibitions against the use of modern slavery and trafficked labour in our contracts with third parties. Using our risked based approach, we will also assess the merits of writing to suppliers requiring them to comply with our Code of Conduct, which sets out the minimum standards required to combat modern slavery and human trafficking.
-
- Consistent with our risk-based approach we may require:
-
- Employment and recruitment agencies and other third parties supplying workers to our organisation to confirm their compliance with our Code of Conduct.
-
- Suppliers engaging workers through a third party to obtain that third parties’ agreement to adhere to the Code.
-
- Consistent with our risk-based approach we may require:
-
- As part of our ongoing risk assessment and due diligence processes, we will consider whether circumstances warrant us carrying out audits of suppliers for their compliance with our Code of Conduct.
-
- If we find that other individuals or organisations working on our behalf have breached this policy, we will ensure that we take appropriate action. This may range from considering the possibility of breaches being remediated and whether that might represent the best outcome for those individuals impacted by the breach to terminating such relationship.
Version Control
| Document Author | David Englefield |
| Document Approver | Dr Adeolu Arikawe |
| Staff Group Consultation | Safeguarding Leeds |
| Version | V1.0 |
| Date Issued | May 2025 |
| Review Date (should be in annual review) | April 2026 |
| Reason for review | New Policy |
Appendix 1 – applicable to SPCL
Modern Slavery Annual Statement 2025 – 2026
Organisational Structure and Supply Chains
SPCL is a provider of Healthcare, whose registered office is in Leicester
We deliver healthcare services in Leicestershire and Warwickshire. We employ staff ranging from General Practitioners, NMC registered Nurses and administrative support staff.
We procure goods and services from a range of providers. Contracts vary from small one-off purchases to service contracts. Our current Procurement processes are as below:
-
- All spend, aside from a few exceptions such as rates, is paid via PO. The Applicable Contract Terms Policy applies to any NHS organisation and states that where an NHS body issues a PO the standard Terms & Conditions apply.
Our procurement process has been reviewed to ensure that human trafficking and modern slavery issues are considered at an early stage, requiring self-certification from potential suppliers that their supply chains comply with the law. We procure many goods and services through frameworks endorsed by the NHS, under which suppliers such as Crown Commercial Services and NHS Supply Chain adhere to a code of conduct on forced labour. We operate professional practices relating to procurement and supply and ensure procurement staff attend regular training on changes to procurement legislation.
Due Diligence Processes for Slavery and Human Trafficking
With regard to national or international supply chains, our point of contact is always preferably with UK entities, and we expect these to comply with legislation and have suitable anti-slavery and human trafficking policies and processes in place. The majority of our purchases utilise existing supply contracts or frameworks which have been negotiated under the NHS Standard Terms and Conditions of Contract, these all have the requirement for suppliers to have suitable anti-slavery and human trafficking policies and processes in place.
Organisational policies in relation to slavery and human trafficking
We update relevant policies on a regular basis to highlight obligations where any issues of modern slavery or human trafficking might arise, particularly in our procedures for safeguarding adults and children and young people, tendering for goods and services, and recruitment and retention.
Assessing and managing risk and due diligence processes in relation to slavery and human trafficking
We are committed to ensuring that there is no modern slavery or human trafficking in our supply chains or in any part of our business. To identify and mitigate the risks of modern slavery and human trafficking in our own business and our supply chain we:
-
- adhere to the National NHS Employment Checks / Standards (this includes employees UK address, right to work in the UK and suitable references
-
- have systems to encourage the reporting of concerns and the protection of whistle blowers
-
- purchase a significant number of products through NHS Supply Chains, who’s ‘Supplier Code of Conduct’ includes a provision around forced labour. Other contracts are governed by standard NHS Terms & Conditions. High value contracts are effectively managed, and relationships built with suppliers.
Effective action taken to address modern slavery – Performance Indicators
We are committed to social and environmental responsibility and have zero tolerance for Modern Slavery and Human Trafficking. Any identified concerns regarding Modern Slavery and Human Trafficking are escalated as part of the organisational safeguarding process. This statement is made pursuant to section 54(1) of the Modern Slavery Act 2015 and constitutes BWPCAs slavery and human trafficking statement for the current financial year.
Training for staff
All staff receive a comprehensive induction programme which includes information on, and guidance regarding, slavery and human trafficking. All staff are required, as part of mandatory training, to complete safeguarding courses, which cover obligations under the Act. We also require external agencies supplying temporary staff to demonstrate compliance with the legislation. All clinical and non-clinical staff have a responsibility to consider issues regarding modern slavery and incorporate their understanding of these into their day-to-day practices.
All colleagues have a personal responsibility for the successful prevention of slavery and human trafficking with the procurement department taking responsibility for overall compliance.
A quarterly Integrated Learning Report is submitted to the Board of Directors which includes an overview of the number of concerns raised by staff and the category that they fall into.
Signed
David Englefield – Managing Director
Dr Adeolu Arikawe – Clinical Lead
Repeat Prescriptions
Introduction
The purpose of this policy document is to set out the methods by which a repeat prescription will be issued and the roles and responsibilities within the practice.
There are Four Stages:
- Initiation/ Request
- Production/ Authorisation
- Clinical control/ Review
- Management control
The GP should retain an active involvement throughout the repeat prescribing process and should not delegate any entire part of the process to ancillary staff. Those stages in bold above are entirely the responsibility of the GP.
Initiation/ Request
The decision to transfer a drug from an acute prescription to a repeat prescription must always be made by the doctor after careful consideration of whether the drug has been effective, well-tolerated and is required long-term. (The patient should be seen, or at least spoken to, at this stage to ascertain this and check compliance). It is the duty of the doctor at this stage to ensure the patient understands the repeat prescribing process and what is required of them.
- Care should be taken to ensure the repeat record is accurate, quantities for each drug are synchronised where possible and review dates are entered. See Appendix A for a synchronisation form which may be handed to the patient to complete.
- Computerisation of repeat prescribing is to be encouraged and is the ultimate aim for all practices
- Drugs should be linked by read code to medical conditions within the clinical system as appropriate.
- Consideration should be given to alternative drugs and / or generic prescribing where appropriate.
Request
- This will largely be the responsibility of the patient.
- The patient should be given a list of drugs they are currently taking on repeat prescription, preferably as a computer-generated list (usually forming the right hand side of the prescription slip).
- The patient or his/her representative must have an active role in requesting a repeat prescription. The patient should be encouraged to indicate on the repeat request slip which drugs they require when a request is made. If they have left the form blank and it is not obvious from their computer record which medication is needed, then the patient should be contacted if possible, rather than all the medication given.
- Only urgent telephone requests or telephone requests from elderly and housebound patients can be taken. Patients should allow 48 hours for requests to be dealt with. This allows adequate time for a good quality repeat prescribing system to operate. For postal requests, to be returned via an SAE, patients should allow one week.
- Patients should be encouraged to tell their GP’s if they are no longer taking a repeat medication. The appropriateness of this can then be assessed and the computer updated to reflect the change.
- It is becoming more common for chemists to request repeat medication on behalf of patients. Whilst this has advantages it is worth bearing in mind that not all chemists check with the patient their monthly needs which can result in everything being ordered when it is not necessarily required. Spot checks with patients and chemists are advisable to ensure the correct dosage and issue of medication is being made to those patients.
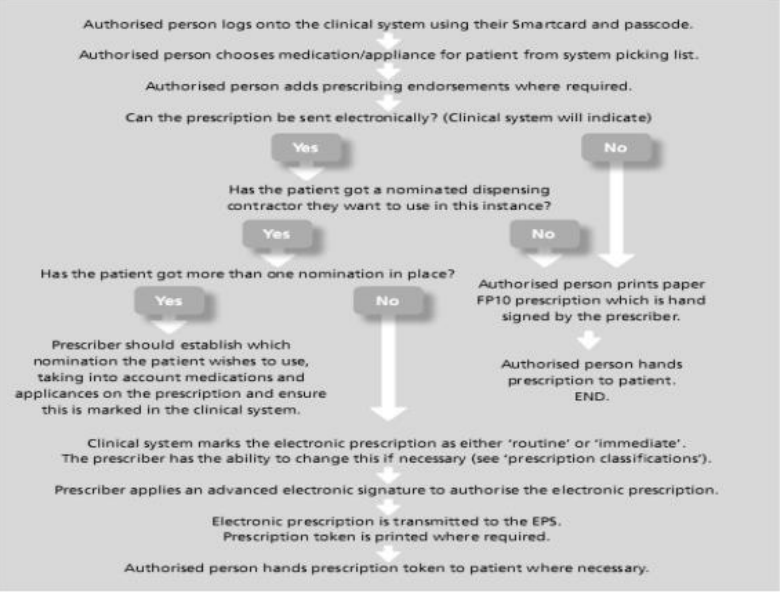
Electronic Prescribing Service (EPS)
This is a new service that is intended to make it easier for GPs to issue prescriptions and more convenient for patients to collect their medicines.
Using EPS means that prescriptions by GPs and other prescribers will be transferred electronically to the pharmacist nominated by the patient. The prescriptions will also be sent automatically to the Prescriptions Pricing Authority (PPA).
A protocol for managing EPS within a practice could be as follows:
Production/ Authorisation
Production
This will usually be the responsibility of the receptionist/prescription clerk.
Computer generated repeat prescriptions are good practice in that handwritten forms are prone to error.
A compliance check is preferable at this stage and the computer should normally alert the user if medication appears to be over or under used. Particular attention should be paid to ‘as required’ drugs and if problems are suspected the doctor should be alerted, preferably before the prescription is produced.
Practices should not supply further repeat prescriptions at shorter time intervals than have been authorised without agreeing the reason for the early request, e.g. holiday and documenting this reason in the patient’s medical record.
Provided there appears to be no problem, a prescription can be generated and left for the doctor to authorise and sign, with the notes to hand (computerised or manual) as far as practically possible, to cross check the validity and appropriateness of the request. Situations where notes should always be available include:
- Where the request slip indicates that a review is necessary
- Where any drug requested by the patient is not on their repeat record
- Where any of the following drugs are requested:
- Temazepam
- Diazepam (Valium )
- DihyGPocodeine
- Paracetamol and codeine 500/30 preparations, e.g. Solpadol,
Tylex - PPI
- All controlled drugs
- Any request about which the practice staff are concerned or uncertain.
- Where additions or corrections are made the doctor signing the prescription should initial or countersign against them. A record should be made of any subsequent handwritten alterations to computer-generated prescriptions.
- Blank prescriptions should never be signed by a doctor for later completion by him/herself or a delegate. To do so is in breach of terms of service.
- Unused space should be cancelled out under the last drug by a computerised mechanism or by the doctor deleting the space manually.
- All repeat prescriptions issued should be recorded on the computer.
- Practices should store prescriptions awaiting collection in a secure way and have a standard time limit for collection of repeat medication (e.g. four weeks) after which those not collected should be investigated, e.g. no longer required or medication underused etc., and then destroyed and noted in the patient’s medical record.
- It may be that patients need their medication to be placed in blister packs of 7 days. This is usually appropriate for elderly patients and those that have serious difficulties managing their medication. A request should be put in to the surgery by either the chemist, district nurse or support worker and this should be passes to a GP for approval. It is then usual to produce these prescriptions in 7 day dosages and 4 can be issued at any one time. Care must be given if a medication is switched part way through a prescription that the dossette boxes are also changed.
Clinical Control/ Review
- This is solely the responsibility of the doctor, although the nurse can review certain patients on behalf of the doctor, e.g.: contraception and asthma although patients may not necessarily have to be seen by the doctor. The review date is set on the computer for every 6 months. For those patients who need annual review, e.g. chronic stable conditions, reviewing them in their birthday month may serve to remind patients of their obligation to attend for review.
- A maximum of 28 days will be given for a prescription. A few patients could be given three month’s supply at GPs discretion e.g. when going on holiday or for certain types of medication – Oral contraceptives, HRT.
- When patients are on several regular long-term medications, quantities should be prescribed to synchronise repeat intervals. In the UK patient packs are moving towards multiples of 28 days (rather than 30)
- When patients are discharged from hospital, their regular medication may have changed. This is a particularly vulnerable time for errors to occur and ideally the doctor should amend the repeat record personally. A check of prescriptions not yet collected should also be made to ensure that it contains the correct medication.
The following considerations should be kept in mind by the doctor when carrying out medication review consultations:
- Control of the condition – is this optimal?
- Unnecessary medication – can anything be stopped?
- Compliance
-
- Is the patient taking the medication properly?
-
- Could the regimen be simplified?
-
- Is there a problem with unwanted adverse effects?
-
- Check understanding of medication?
-
- Monitoring – is this required, e.g. phenytoin levels, INR, TFTs, LFTs, U&Es
- Cost considerations – change to generics if appropriate, or consider change to a more cost-effective treatment (consider local formulary)
Management control
This would largely be the responsibility of the practice manager.
Practice staff that write, or are involved in the preparation of, repeat prescriptions should be appropriately trained in the practice protocols for repeat prescribing, what their responsibilities are, and the need for accuracy. This should be on going, but is particularly important for new staff.
Liaison with local community pharmacists is essential if procedures are changed that may ultimately impact on them.
An adequate system for the secure storage and use of FP10s should be in place. A log sheet will be kept (& maintained by prescription clerk TB) for prescription pads coming into the practice (from PCSE) and distribution within the practice. This will be audited twice every year.
The practice computer system holding the prescribing records must be backed-up regularly.
Periodic audit of repeat prescribing will be carried out annually. This audit should also include prescription re-prints.
Setting up a repeat prescription
The medication to be included on a repeat prescription should be agreed between GP and patient. Certain items should not be on repeat (& should be on acute only). These include (but are not limited to:
- Contraceptive pills
- HRT
- Salbutamol
- Controlled drugs
-
- The importance of the need for regular review of repeat medication should be stressed to the patient.
-
- It is the responsibility of the patient’s GP to ensure that an accurate up-to-date record of a patient’s repeat medication is held in their computer records and that all prescriptions are indicated / linked to a condition by read code.
-
- Repeat medication prescriptions should last for an agreed length of time, usually 6-12 months, before medication should be reviewed (although this period can be extended if felt appropriate at the discretion of the prescribing GP).
-
- Provide patients with details of the system operation at an appropriate time (on registration with the practice, on commencing a repeat prescription). Posters detailing the operation of the system should be displayed around the practice.
Operation of the system
The practice staff are responsible for the day to day running of the system. This should include:
- An appointed member of staff being given responsibility for the daily collection and processing of all repeat prescription requests.
- When preparing a repeat prescription, practice staff can make brand to generic name switches as appropriate (see attached list of those medications which should only be prescribed by brand name).
- Routine reauthorisation of repeat prescriptions is the responsibility of the Doctor. If items requested have expired and need reauthorisation the patient is required to attend a medication review, unless housebound. If housebound, the GP is then responsible for deciding whether to automatically re-authorise the repeat prescription or to provide a home visit.
When to refer the prescription back to the doctor
If anything is unclear with a repeat prescription request refer back to the prescribing GP.
If a patient requests an item which is not included or differs from the details recorded in their records, they should be referred to the GP.
If a patient under or over orders items on their repeat prescription indicating poor compliance, this should be highlighted with the GP.
Monitoring of repeat prescribing
Ideally a GP should carry out a medication review when:
- A block of repeat medication comes to an end.
- Patients attend for monitoring of the condition requiring repeat treatment.
- Opportunistically should a patient attend with another complaint
The review should consist of an assessment of the patient’s condition and compliance with prescribed medication. If any repeat medications are no longer being requested, an attempt should be made to ascertain the reason why and appropriate action taken.
Controlled Drugs
All controlled drugs not sent electronically (EPS) should be signed for by the person collecting the prescription e.g. patient / chemist.
Appendix B shows the signature form
Non-collection of prescriptions
Monthly checks will be carried out of prescriptions not collected (by the prescribing clerk). Prescriptions will be cancelled on the patient’s prescribing record & a note added. The prescribing clerk will task the GP to advise them that a prescription has not been collected & what details of the medication. The GP will then decide if any action needs to be taken i.e. follow up call / consultation if concerns (mental health patient etc.)
Repeat Prescribing Flowchart
Following agreement between patient and doctor to commence medication on a repeat prescription: 
Summary Care Record
There is a new Central NHS Computer System called the Summary Care Record (SCR). It is an electronic record which contains information about the medicines you take, allergies you suffer from and any bad reactions to medicines you have had.
Why do I need a Summary Care Record?
Storing information in one place makes it easier for healthcare staff to treat you in an emergency, or when your GP practice is closed.
This information could make a difference to how a doctor decides to care for you, for example which medicines they choose to prescribe for you.
Who can see it?
Only healthcare staff involved in your care can see your Summary Care Record.
How do I know if I have one?
Over half of the population of England now have a Summary Care Record. You can find out whether Summary Care Records have come to your area by looking at our interactive map or by asking your GP
Do I have to have one?
No, it is not compulsory. If you choose to opt out of the scheme, then you will need to complete a form and bring it along to the surgery. You can find a copy of the form here: SCR Opt Out Form
More Information
For further information visit the NHS Digital website.
Telephone Recording
All telephone calls to and from the surgery are recorded to protect our patients and healthcare professionals. Patients are protected by the practice having a record of our conversations with patients, staff and other health workers to protect from potential abuse. We also occasionally use recordings for staff training and quality control.
For new patients, when you register with us, we will make it clear that all inbound and outbound calls from the surgery are recorded.
Calls, or transcripts of calls, audio or audio-visual recordings or elements of the discussion you have with the clinicians that contain clinical information may be added to your medical records, but this will be clarified with you at the time.
The recordings are stored securely on a system provided by X-on and are protected through the company’s Data Protection Policy, which is complaint with GDPR legislation. These recordings will not usually be shared outside the practice. If we hold recordings that have not been deleted, you can ask for a copy. In order to do this, you must put the request in writing to the Practice Manager via a Subject Access Request.
Violent and Abusive Patients
The practice will not tolerate violent or abusive behaviour.
Anyone verbally abusing either a member of staff or the public, or using inappropriate language, will be asked to leave the premises and requested to find another GP.
Anyone who is violent or causes damage will be removed from our list immediately.
Patients will also be removed from the list in the following circumstances:
- Violence and aggression towards staff or members of the public;
- Damage to practice property or equipment;
- Change of residence to outside of the practice area;
- Persistent misuse of the system; or
- Patients who the doctors are unable to manage clinically e.g. breach of contract with doctor regarding use of prescribed medicine, break down in patient communication.
Members of our team are instructed to dial 999 for police assistance if patients are disruptive and display aggressive and/or intimidating behaviour and refuse to leave the premises when asked. Charges may then be brought against these individuals.
Your Personal Health Information
We ask you for information and keep it together with details of your care.
We may use some of this information to help us to protect the health of the Nation, to help plan the future of the NHS, to train tomorrow’s clinical staff and to carry out research for the benefit of everyone.
You have a right of access to your health records. Please ask at reception for further details.
Everyone working for the NHS has a legal duty to keep information about you confidential.